PTSD is treatable! Veterans, it’s time to seek help
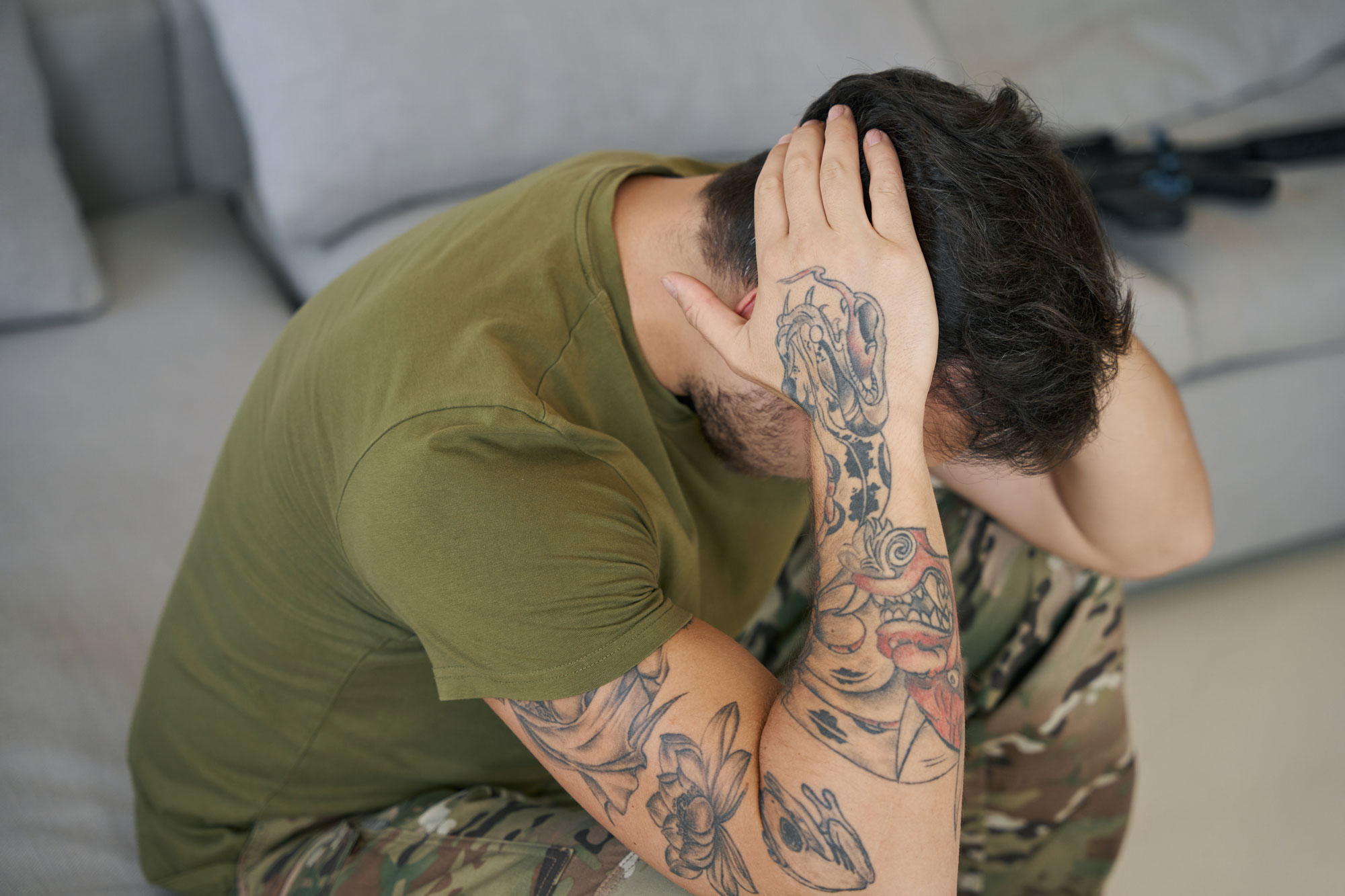
Since 2001, more US troops have died from suicide than were killed in Afghanistan. The Army estimates that up to 20 percent of soldiers who were deployed in Iraq and Afghanistan – 500,000 men and women – will suffer from disabling agitation, nightmares and emotional withdrawal – all signs of post traumatic stress.
Approximately 19 million veterans live in our country today; and about 20 percent have a mental health issue – from PTSD to depression, bipolar disorder and substance abuse – and the more intense their combat exposure was – the higher risk they are of suicide. According to one government estimate, 17 veterans die by suicide every single day. Male veterans are 1.5 times more likely to die by suicide than civilians, and female veterans are 2.2 times more likely to die by suicide than civilians.
The Department of Veterans Affairs projects a 32 percent spike in outpatient mental health care for veterans over the next 10 years. One third of these individuals have been diagnosed with at least one mental health concern.
PTSD is not new; Civil War soldiers suffered severe psychological distress, and more than one million World War II veterans displayed signs. Finally, in 1980, the American Psychiatric Association named the condition Post Traumatic Stress Disorder (PTSD), a very real mental health issue.
A big concern is that, even though this condition has been recognized, very little will change when it comes to members of the military and veterans seeking help.
What happens after trauma exposure?
Military personnel often have recurring thoughts of the event and frequent nightmares, and these can trigger a number of physical reactions. In many instances, the experiences will fade away, but often they linger on for weeks, months and even years, and can impact relationships and interfere with everyday life. Depression, anxiety, avoidance, guilt, shame and lack of trust all are signs of trauma. Its frequency, intensity and duration all can contribute to PTSD.
It is estimated that about 12 percent to 17 percent of members of the military and veterans will have PTSD.
What makes PTSD worse?
- Avoidance: Not talking about what happened can worsen PTSD.
- Isolation: Many will hide out and stop socializing, which also worsens PTSD.
- Trying not to think about the traumatic event: the more you try not to think about it, the more you will think about it. The harder you try to bury the memory, the more it will resurface.
- Being on “guard duty” 24 hours a day: you may feel you have to guard your home by responding to every noise you hear.
Here are a few myths about PTSD:
- PTSD is untreatable. FALSE.
- PTSD is a lifelong condition. FALSE.
- Situations that are reminders of the trauma should be avoided. FALSE.
- Other people have traumas worse than you so you don’t need to seek help. FALSE.
- Treatment is dangerous and can worsen the condition. FALSE.
- Seeking help is a sign of weakness. FALSE. It’s time to give up this stigma. Many members of the military and veterans have PTSD because they were strong enough to face some of the most difficult challenges of their life and witness horrific events.
I understand that seeing a therapist can be embarrassing, humiliating and socially stigmatizing. It also can affect your career in the military as well as your standing and clearances. At least half of all active duty persons and veterans diagnosed with PTSD and major depression do not seek therapy; many worry this information will go on their permanent military record.
However, seeking help from a therapist not connected to the military system is not required to be reported.
As a veteran who served in the United States Air Force, I understand military culture, I grew up surrounded by veterans in my family, I lived that culture. Even though I am a mental health therapist, military culture is embedded in me; it is part of who I am today.
I watched 18 year-olds in charge of top secret information and the pressure they were dealing with; I learned of a caravan bombing where many soldiers died, and those who survived were offered no mental health support; I was pregnant during my time in the Air Force, and I experienced the trauma of extreme verbal abuse and mistreatment because of my pregnancy. These are three of many stories I can share about the military and how there were no coping mechanisms offered for dealing with some of the most horrific experiences in our lives.
My rule of thumb is this – if you are thinking you need therapy, you should go; if you are not thinking about therapy, you most likely will need it. Do not give into the darkness. Talk to a professional.
Remember, it is not a sign of weakness to seek therapy.
In addition, the transition from military life to civilian life can bring a whole different set of challenges. Many veterans are focused on adapting to a new career and its changes and may not acknowledge that they need therapy. For example, those who sought help after 9/11 is about half the number of those who need help.
That’s why finding a good mental health therapist is critical. Ask yourself these questions:
- Does the person you are planning to see have the background and understanding to help you?
- Does the therapist understand the stigma that comes with serving in the military?
- Does the therapist understand military culture or anything about the military?
- Has the therapist worked with veterans before?
If you want to seek help but feel you don’t need it or are reluctant to acknowledge that you cannot handle your problems on your own, consider the following:
- Because of the stoic mindset veterans absorbed in the military, it may be hard to ask for help. A normal “go to” response is to power through your issues alone, but has this been working so far?
- When a sense of community is lost upon leaving the military, it can be an alienating experience. The military is a very tight knit, connected group. You are willing to die for another person or your country. These people become your family. When you return home, you may feel a loss of purpose and struggle to find meaning in your life again.
- Your sense of self takes a hit. After years in uniform and being addressed as “ma’m,” “sir,” “Major,” etc, this is engrained in your daily life. When this disappears, your sense of self can be negatively impacted.
- My advice: take charge of your mental health. Find a professional who has experience working with veterans and take one step at a time. Call me. I’ll give it to you straight! You can be yourself with me.
